The Ultimate Guide to Postpartum Care (From Underwear to Hair Loss)
There is a lot of support for mothers and birthing parents during the prenatal period, but postpartum care looks a bit different. Upon leaving the hospital following childbirth, you will be armed with supplies like maxi pads, diapers, and witch hazel wipes but may be feeling a little uncertain, overwhelmed, and uncomfortable as you embark on the next journey — the fourth trimester.
Depending on complications following childbirth or a cesarean section, you may see your gynecologist a few days after your baby is born, but after that, you will most likely not have another visit until you are 6 weeks postpartum. New moms and parents can prepare for the postpartum period and encourage a smooth postpartum recovery by knowing what to expect. While the new baby's health is most attended to, a mother or birthing parent's well-being is just as important. As much as a birth plan can help ease your nerves, communicate to your birthing team your needs and wants, and give you an idea of what might happen in the delivery room, things do not always go to plan, so it's important to know what to expect in all situations.
Our complete guide to postpartum care can help moms, dads, and other birthing parents plan for life after the birth of a baby, to help everyone get as comfortable as possible amid this big life-changing transition.
What to Expect After Vaginal Delivery
After a vaginal delivery, you will experience lochia, or vaginal bleeding and discharge that at times may be similar to a menstrual period. Soreness of the vaginal area will continue for days after a vaginal delivery and can be managed with prescribed or over-the-counter pain medication as needed. If your perineum tears or you need an episiotomy, your doctor will apply dissolvable stitches to the area afterward.
After delivering the baby and the placenta, there's still a lot more material that needs to come out. To assure your uterus is emptied, for the first couple of hours, your nurse will come in frequently to massage your stomach with pressure, to force remaining substances out of your uterus. This can cause some additional pain. Medication will be prescribed to you while in the hospital and to take when you return home to reduce postpartum pain levels. After a vaginal delivery, you should not have sex for four to six weeks postpartum to allow for full healing.
What to Expect After a C-section

C-section births require more healing time and a longer stay at the hospital, due to an incision being made in your lower abdomen for the baby to be born. You should have an additional appointment with your obstetrician around three weeks out to check your healing progress. Like with vaginal delivery, after a c-section, you will have lochia bleeding and discharge from your vagina, but it should be less heavy than that of a vaginal delivery. However, you have additional care needs during this method of birth.
Upon returning home, rest is important, and you should limit the number of stairs you go on, and not lift anything heavier than your baby's weight. The area where your baby is removed during surgery will be stitched up, and keeping it clean and dry at all times is crucial to recovery. If you notice redness, swelling, or discharge at the incision site, or are running a fever, contact your healthcare provider, as this could be a sign of infection. Full recovery takes about six weeks on average, though this varies person-to-person, and you should abstain from sex for this time period in order to safely and fully heal.
Breastfeeding Timeline and Tools

Immediately after your baby is born, or just before, you will begin to make colostrum, a golden liquid preceding milk that will be your baby's first meal outside of the womb the first two to five days of their life. Following this, milk tends to come in between days three and five, though some factors can make it show up later, including heavy bleeding from birth, stress, thyroid conditions, prenatal bed rest, and other health conditions. If you wish to continue body feeding or breastfeeding, the beginning period may present challenges and require patience to get into a routine with it.
Breast milk supply tends to be based on demand, so the more you nurse or pump postpartum, the more breast milk you will make to meet your baby's needs. But this can be impacted by things like medication, latching problems, duct infections, and a feeding parent's mental health.
New moms and nursing parents may have to speak with multiple lactation consultants in the hospital and hear different recommendations, which can lead to confusion. When baby first comes home, they may have the desire to cluster feed, which consists of nursing repeatedly for many hours. Apps may be helpful for tracking the times your baby is nursing, so you can keep your pediatrician and your chosen lactation consultant informed.
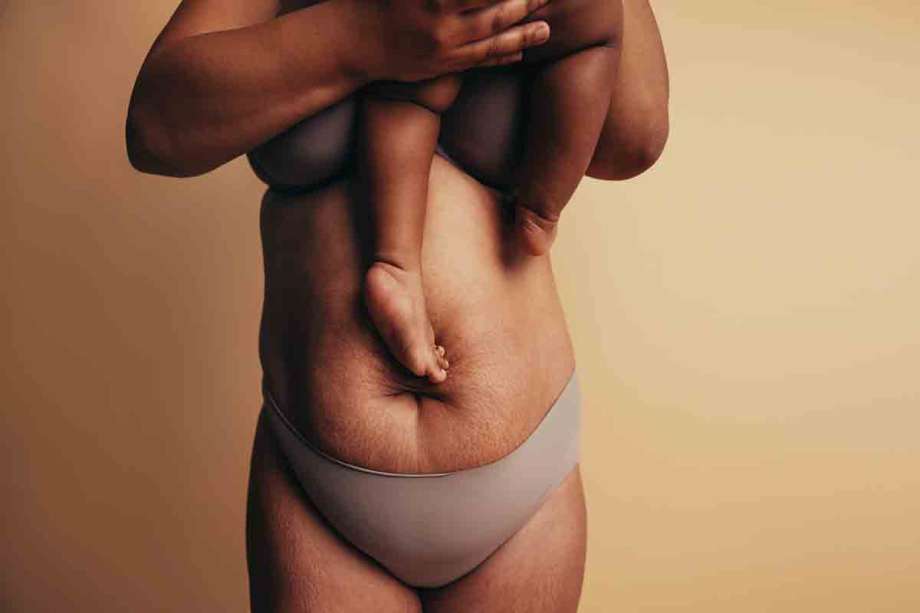
Postpartum Weight-Loss
It may take a long time for your body to go back to its normal size (if it ever does). But according to the Mayo Clinic, the average person sheds around 13 pounds immediately following birth. Other weight that you may have gained can take longer to come off, and factors like breastfeeding may either help with weight loss or contribute to weight gain, depending on the person.
Your health care provider can give you advice for a healthy diet and exercise at each stage of your postpartum time. Your goal should be to eat a balanced diet with fruits, vegetables, protein, calcium, and other nutrients, adding more calories depending on your activity level. Depending on your birth and pregnancy complications, you may have to wait a while before doing strenuous activity. It's important to move when it's safe to do so, starting out slowly with walks and gradually increasing your level of activity as you recover.
Postpartum Hair Loss
While your hair may be long and voluminous amid pregnancy, in the postpartum phase, all that extra growth may start to follow out. Postpartum hair loss is normal. Excessive hair shedding typically continues for about four months. With a high amount of hair loss, be sure to pay attention to your baby's fingers and toes. Your hair can get stuck on their extremities, as strands can wrap around and lead to a hair tourniquet that can cause problems for your child. Inspect their feet before putting them into footed pajamas or socks.
To feel better about your hair, you may need to rethink your beauty routine. Avoiding heavy hair products, high heat styling, and lowering your brushing frequency can all help reduce the loss of hair. A haircut can add volume to your hair if you are facing heavy hair loss. By the time your child turns one, your hair should be back to normal in terms of loss, though texture change can happen during pregnancy that may be permanent. If you are concerned about your hair loss, contact your obstetrician or dermatologist.
Helpful Products for Postpartum Recover at Home

Some postpartum products can help new moms and birthing parents be more comfortable and heal more quickly after having their baby. A sitz bath is designed to help you soak your genital area with warm water postpartum. This device sits in your toilet so you can easily use it. It can help soothe (especially if you have perineum tearing from birth or an episiotomy), keep the area clean, and promote healing. Another tool to help keep the vaginal area clean is a peri rinse bottle, used to shoot water in your vaginal area every time you use the restroom. Baby wipes are good to have on hand for yourself as well, as toilet paper can be irritating and get caught on stitches during the healing process.
Heating pads placed on your back and lower abdomen can help soothe for postnatal cramping. Heavy bleeding will occur for up to ten days, so you'll want sterile protection in that first week. While your hospital will provide large maxi pads and ice packs to place in your underwear to soothe the sore area, some people are more comfortable in an adult diaper after birth or their favorite brand of unscented pads. Tampons and menstrual cups should not be used, as they can lead to an infection in the postpartum period and slow healing.
Sex, Birth Control, and Periods Postpartum
Following most pregnancies, doctors advise against having sex again until about four to six weeks postpartum. When you reach the six-week point, you will have a visit where they will most likely clear you to do the deed again, and address any other concerns. Sexual intercourse may be painful due to vaginal dryness and lingering soreness, so take things slowly, and make use of lubricants and pain medication as needed when you are ready. Non-penetrative sex and foreplay may be more comfortable and still a good way to connect with your partner.
If you do not feel up to sex yet at all at this point, do not feel pressured. This time period is when it's safe to do so, but that does not mean it will be the right time for you and your partner to begin again. Find other ways to be intimate with your partner with small moments of quality time.
At this point, you can also go back on birth control, whether that's an estrogen pill, an implant, or an intrauterine device. Note that hormonal birth control can increase your risk of blood clots in the postpartum period. While breastfeeding can provide protection, it is not guaranteed to prevent pregnancy, even before your period returns. If you and your partner want to begin trying for another child, 18 to 24 months is the recommended time frame, though beyond that prior to five years after your first child is considered safe.
Eventually, your menstrual cycle will return, which means you will be ovulating again soon. Factors like stress and whether or not you breastfeed will play an impact on when your period comes back. If you are not exclusively breastfeeding, it should start again between six and eight weeks after your baby is born. In this instance or earlier, tampons are generally not advised during your healing. If you are breastfeeding, the time period your period will return can be extremely varied due to hormone production. Note that pregnancy and birth may change your period. Some women may have lighter, less painful cycles, while others can have heavier bleeding, clotting, irregularity, and cramping.
Postpartum Constipation
As your body begins to heal from carrying and growing a child, and then giving birth, constipation can last throughout the postpartum period. Constipation is normal during and after pregnancy and can continue for weeks after your child's birth. Hemorrhoids are a common cause and symptom and can be treated with witch hazel. The issue may be exacerbated by pain from an episiotomy, anal sphincter damage. Whether your first bowel movement after your child is born happens in the hospital or at home, it may be painful and uncomfortable, but taking certain steps can help make it more bearable.
Be sure to eat a lot of fiber, like leafy green vegetables, fruits, and whole-grain cereals, and drink a lot of fluids to help get things moving. You can also start taking stool softener immediately after your baby is born to help make yourself more comfortable and have less pain when using the restroom. Exercise is also important. Start off with short, daily walks if your doctor says it is safe to do so.
While constipation issues can continue for a while after birth, if you do not have a bowel movement four days after birth, visit your gynecologist. They may recommend a prescription-strength laxative. For severe constipation, also cut back on iron supplements, as they can make the problem worse. It may a while for your bowel movements to become regular again, and stool softener can be continued as much as you need it.
Dealing with Postpartum Depression

Baby blues and mood swings after giving birth are normal for new mothers. Lack of sleep amid such a huge, life-changing transition further increases these feelings. But there are some symptoms of postpartum depression to watch for as you recover that can indicate a mental health issue after having a baby. If you already struggle with mental illness, your risk of developing postpartum depression is much higher.
Despite the stigma against mental health struggles, do not be afraid to ask for help. If you are having thoughts of worthlessness, long-lasting sad feelings, irrational fears about your loved ones or yourself, or thoughts that your baby or family would be better off without you, talk to someone you trust, like a friend, your partner, a doctor, or another family member.
Talk therapy, whether virtually or in person, helps you speak about and deal with what you are feeling with a trusted professional who can help you process trauma related to the birth and find the proper treatment plan. Your child's pediatrician will likely give you a questionnaire for the first few checkups and may be able to help you find a therapist.
Self-care is very important during this time, though it can be difficult to fit into your routine when your baby needs you so frequently. Try to eat three meals a day with nutritional value, drink a lot of water and get some fresh air.
Walks outside will benefit you — and your baby. They will enjoy getting a change of scenery just as much as you, and you will both benefit from your well-being. Take advantage of any help you have, whether it is your partner, friend, or family member. If you do not have a support system, consider hiring help, or finding emotional support online through parent groups or mom friendship applications.
Try not to put pressure on yourself in the first few months to keep your home clean or get everything done. The postpartum period is challenging and can be very difficult physically and mentally. Focus on your healing and time with your baby, and do the best you can with the resources you have. When you become a mother, your life changes, and your routines and perspectives need to adjust as well.

